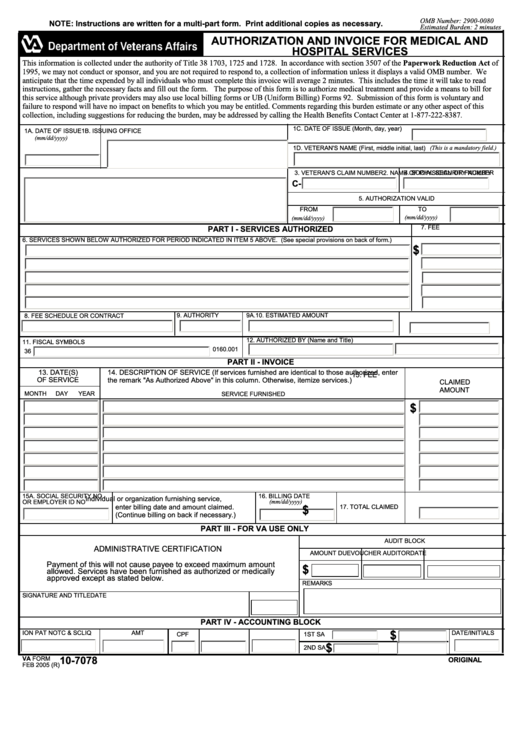
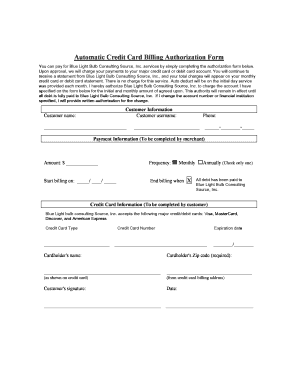
When it comes to revenue cycle management, medical billing is the first thing that helps the organization generate more revenue. an optimized medical billing process is the primary focus to ensure long-term operations. in this way outsourcing medical billing services, enables healthcare organizations to accelerate the pace of revenue generation. Revele gives you everything you need for a high performing revenue cycle operation. contact us today to learn how we’re redefining rcm with an end-to-end ecw rcm solution. As a medical billing professional, dealing with prior authorization is a necessary part of the job. prior authorization (also known as preauthorization) is the process of getting an agreement from the payer to cover specific services before the service is performed. normally, a payer that authorizes a service prior to an encounter assigns an authorization
What does a medical billing agent make?. hospitals, physicians, home health agencies and insurance companies rely on medical billing agents to review claims, verify patients' insurance information, ensure proper payments are allocated and p. This is the newest place to search, delivering top results from across the web. medical billing authorization number content updated daily for billing and coding medical.
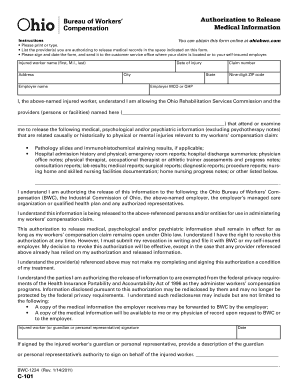
Medical record number, if available; date of service; provider name or facility or clinic name requesting records from; choose method of receipt by clearly indicating the mailing address, fax number, email address or select patient gateway, if available, to send the records to. 3. sign and date the completed authorization form. 4. Take these steps after you find out that your medical bills are now in the hands of a collection agency. find out how you can address it quickly and effectively to ensure that you can pay off this type of debt and avoid long-lasting damage.
Prior authorization (also known as preauthorization) is the process of getting an agreement from the payer to cover specific services before the service is performed. normally, a payer that authorizes a service prior to an encounter assigns an authorization number that you need to include on the claim when you submit it for payment. In medical billing, pre authorization is a pre-approval before providing medical service. an insurance plan requirement in which the service provider must notify the insurance company in advance about certain medical procedures or services in order for coverage to be considered. Get your medical release document today. create legal documents using our clear step-by-step process. We would like to show you a description here but the site won’t allow us.
Feb 17, 2020 · medical coding is the step in the medical billing process that assigns codes to insurance claims so that a patient’s insurance can be correctly billed. this system of medical coding ensures that healthcare visits are categorized correctly when it comes time to bill and process insurance claims. New medical providers should submit enrollment applications online. should providers need assistance in submitting online applications, please contact: dfec: 1-844-493-1966. dcmwc: 1-800-638-7072. deeoic: 1-866-272-2682. select option 2 (for provider) and then medical billing authorization number select 3 (for enrollment). Do you know how to start a medical billing business? find out how to start a medical billing business in this article from howstuffworks. advertisement by: howstuffworks. com contributors many doctors across the country rely upon medical bil. Jun 29, 2021 · a medical billing solution can reduce the number of employees who would otherwise have been required to manage claims, billing and collections manually. automated entries reduce the number of errors. it improves patient care, improves outcomes and reduces double entry of data.
Information For Medical Providers U S Department Of Labor

Partnership Agreement
Prior authorization is a process through which a request for provisional affirmation of coverage is submitted to a medical review contractor for review before the item or service is furnished to the beneficiary and before the claim is submitted for processing. it is a process that permits the submitter/requester (for example, provider, supplier. Medical expenses can be overwhelming. learn more on how to make sense, manage, and pay off you or your family's medical bills. read full profile according to a u. s. news and world report article, about eight in 10 medical bills contain some. Early submission of authorization request: it is important to submit authorization requests before treatment. early submission helps in obtaining the authorization number to determine the payment. mention authorization number: while processing the claims make sure to include the authorization number to prevent rejection of claims. this establishes that you have received prior authorization. It's not uncommon for people to struggle to pay their medical bills, and it's certainly nothing to be ashamed of. but it's a good idea to be proactive from the outset if you can. here are 10 things you can do to improve your situation.
Providers may request a “stat” authorization (for services that are urgent in nature) by: • calling prestige health choice (have the member’s name, id number, diagnosis and service available when calling) at 888-611-0784. prior authorization general information. Learn how fast healthcare interoperability resources impacts prior authorizations. read our white paper today. A: call the imaging department at 503-571-8451 or fax a completed authorization for kaiser permanente to use/disclose protected health medical billing authorization number information (phi) form to 503-571-8469. remember to sign the authorization in ink. x-ray images can only be released on a cd or dvd. q: how do i have my prior medical records added to my kaiser permanente record?.
The common problem faced by all medical billing companies is long waiting time before the approval of the prior authorization. a recent report from american medical association found that 64% of providers reported waiting for at least 1 business day and 30% reported at least 3 business days. Billing: definitions of commonly used terms; a; a; a; authorization number — a number stating that your treatment has been approved by your insurance plan. medical record number — the number assigned by your doctor or hospital that identifies your individual medical record.. Here's how you can pay medical bills without using credit cards. disclaimer: this site contains affiliate links from which we receive a compensation (like amazon for example). but they do not affect the opinions and recommendations of the a.
Injured workers and providers can check on the status of medical authorizations on the owcp web bill processing portal. to speak with a customer service representative regarding an authorization, you may call 844-493-1966, toll free. this number is available monday to friday, 8am to 8pm, est. Should providers need assistance in submitting authorization requests, please contact: dfec: 1-844-493-1966; dcmwc: 1-800-638-7072; deeoic: 1-866-272-2682 select option 2 (for provider) and then select 2 (for authorizations). the new authorization templates can be found here: dfec authorization templates.